⊡ Introduction to Glaucoma
What Is Glaucoma?
Glaucoma is a serious eye condition that damages the optic nerve, which plays a crucial role in transmitting visual information from the eyes to the brain. This damage is often linked to increased pressure inside the eye, known as intraocular pressure (IOP), though glaucoma can also occur with normal eye pressure. Over time, untreated glaucoma can lead to permanent vision loss or even blindness.
What makes glaucoma particularly dangerous is that it often progresses silently, without noticeable symptoms in its early stages. Many patients remain unaware of the condition until significant vision damage has already occurred. For international patients seeking quality eye care abroad, understanding glaucoma and recognising its early signs is essential. Early diagnosis and treatment can slow or stop disease progression, preserving vision and improving quality of life.
Types of Glaucoma
Glaucoma is not a single condition but a group of eye disorders that damage the optic nerve and can lead to vision loss if left untreated. Each type of glaucoma develops differently and may show distinct symptoms or progression patterns. Understanding these types helps patients recognise warning signs early and seek timely medical care. This awareness is especially important for international patients considering eye treatment abroad.
Primary Open-Angle Glaucoma
Primary open-angle glaucoma is the most common form of the disease and develops gradually over time. It usually causes no pain or noticeable symptoms in the early stages, making regular eye exams essential. Vision loss typically begins with peripheral or side vision and slowly progresses toward central vision. Many patients remain unaware of the condition until significant damage has already occurred.
Angle-Closure Glaucoma
Angle-closure glaucoma occurs when the drainage angle of the eye suddenly becomes blocked, causing a rapid increase in eye pressure. This type often presents with severe symptoms such as eye pain, headaches, blurred vision and halos around lights. Unlike open-angle glaucoma, symptoms appear quickly and worsen rapidly. It is considered a medical emergency that requires immediate treatment to prevent permanent vision loss.
Normal-Tension Glaucoma
Normal-tension glaucoma is a type where optic nerve damage occurs despite eye pressure remaining within normal ranges. The exact cause is not fully understood, but it may be related to reduced blood flow to the optic nerve. Vision loss develops slowly and may go unnoticed in the early stages. Regular monitoring is crucial for early detection and management.
Secondary Glaucoma
Secondary glaucoma develops as a result of another medical condition or external factor affecting the eye. Causes may include eye injuries, inflammation, tumors, or prolonged use of steroid medications. The increase in eye pressure can occur suddenly or gradually depending on the underlying cause. Treating both the glaucoma and its root cause is essential for effective management.
Congenital Glaucoma
Congenital glaucoma is a rare condition present at birth or appearing in early childhood. It occurs due to abnormal development of the eye’s drainage system, leading to increased eye pressure. Symptoms may include enlarged eyes, excessive tearing and sensitivity to light. Early diagnosis and prompt surgical treatment are vital to protect the child’s vision.
⊡ Understanding the First Signs of Glaucoma
The first signs of glaucoma are often mild and easy to miss, particularly in open-angle glaucoma, the most common form of the disease. Vision changes usually develop slowly and without pain, allowing the condition to progress unnoticed for years. Because central vision remains normal in the early stages, many people do not realise their eyesight is being affected until significant damage has occurred. Early awareness of symptoms is essential to prevent permanent vision loss.
Gradual loss of peripheral (side) vision
One of the earliest signs of glaucoma is a gradual narrowing of side vision. This change usually occurs so slowly that patients may not notice it at first. Over time, reduced peripheral vision can affect activities like walking, driving, or navigating crowded areas. Without treatment, the vision loss continues to progress inward toward central vision.
Difficulty seeing in low-light conditions
Early glaucoma can make it harder for the eyes to adjust to dim or dark environments. Patients may struggle with night driving or moving from bright to dark areas. This occurs due to damage to the optic nerve affecting visual sensitivity. Such difficulties are often mistaken for normal aging rather than an eye disease.
Bumping into objects or misjudging space
As side vision decreases, individuals may begin bumping into furniture or doorways. Depth perception and spatial awareness can also be affected over time. These signs often appear gradually and are commonly ignored. Many patients only recognise the problem after repeated incidents.
Sudden eye pain and severe symptoms (angle-closure glaucoma)
Angle-closure glaucoma causes a rapid rise in eye pressure, leading to intense eye pain and discomfort. Symptoms may include headaches, nausea, vomiting and severe blurred vision. Halos around lights are also commonly reported. This form of glaucoma is a medical emergency requiring immediate treatment.
Blurred vision or seeing halos around lights
Some patients experience blurred vision or notice bright halos around lights, especially at night. These symptoms may occur during sudden increases in eye pressure. Vision can worsen quickly if not treated promptly. Immediate evaluation by an eye specialist is essential to prevent permanent damage.
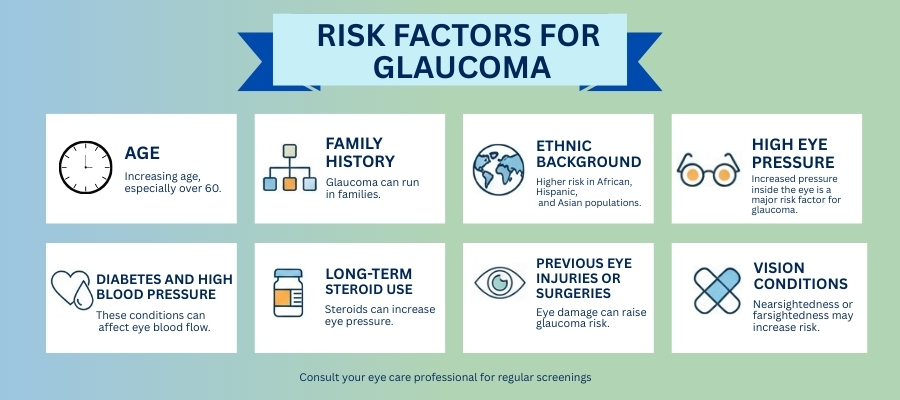
⊡ Risk Factors for Glaucoma
Glaucoma does not affect everyone equally, and certain factors significantly increase a person’s risk of developing the condition. Many people with glaucoma are unaware of these risk factors until vision damage has already occurred. Understanding who is more vulnerable helps promote early screening and preventive eye care.
For international patients, awareness of glaucoma risk factors is especially important, as access to routine eye exams may vary across countries. Knowing personal risk factors allows individuals to seek timely evaluation and treatment, even before symptoms appear, reducing the chance of permanent vision loss.
Age
Advancing age is one of the strongest risk factors for glaucoma. People over the age of 40 have a higher likelihood of developing the condition, with the risk increasing significantly after age 60. Age-related changes in eye structure and drainage can raise eye pressure over time. Regular eye exams become increasingly important as people grow older.
Family History
A family history of glaucoma greatly increases the risk of developing the disease. If a parent or sibling has glaucoma, the chances of optic nerve damage are much higher. Genetic factors play a key role in how the eye handles fluid pressure. Individuals with affected family members should begin eye screening earlier and undergo regular monitoring.
Ethnic Background
Certain ethnic groups are more prone to specific types of glaucoma. People of African descent are at higher risk for open-angle glaucoma, while Asian populations are more susceptible to angle-closure glaucoma. Hispanic individuals also face an increased risk as they age. Understanding ethnic susceptibility helps guide early diagnosis and prevention strategies.
Diabetes and High Blood Pressure
Chronic conditions such as diabetes and high blood pressure can increase the risk of glaucoma. These diseases affect blood flow and may damage the optic nerve over time. Poor circulation can make the optic nerve more vulnerable to pressure-related damage. Managing these conditions plays a vital role in protecting long-term eye health.
Long-Term Steroid Use
Prolonged use of corticosteroids, especially steroid eye drops, can raise intraocular pressure. Some people are particularly sensitive to steroids and experience pressure increases even with short-term use. This type of pressure rise may go unnoticed without monitoring. Patients using steroids should have regular eye pressure checks.
Previous Eye Injuries or Surgeries
Eye injuries, surgeries, or severe infections can disrupt the eye’s natural drainage system. This disruption may cause fluid buildup and increased eye pressure over time. Secondary glaucoma can develop months or even years after the initial injury. A history of eye trauma should always be shared with an eye specialist.
Vision Conditions (Nearsightedness or Farsightedness)
Extreme nearsightedness or farsightedness can increase the risk of certain types of glaucoma. Farsighted individuals are more prone to angle-closure glaucoma due to eye structure differences. Nearsightedness may be associated with open-angle glaucoma. Regular eye exams help monitor these structural risks.
For international patients, providing a complete medical and eye history during consultations abroad is essential. A thorough understanding of personal risk factors allows specialists to create accurate diagnosis plans, choose the most effective treatments and ensure long-term vision preservation.
Age, family history, and underlying health conditions can silently increase your risk of glaucoma. Many people develop the disease without realising they are vulnerable. Delaying eye check-ups allows damage to progress unnoticed. Knowing your risk early can help protect your vision for life! ”
⊡ Diagnosing Glaucoma
Common Diagnostic Tests
Diagnosing glaucoma requires a series of specialised eye tests rather than a single examination. One of the most common tests is tonometry, which measures eye pressure. An optic nerve examination allows the doctor to check for visible damage.
A visual field test evaluates peripheral vision loss, while optical coherence tomography (OCT) provides detailed images of the optic nerve and retina. These tests help detect glaucoma early, even before symptoms appear.
For international patients, advanced diagnostic technologies available at specialised eye centers abroad ensure accurate detection and timely intervention.
Importance of Regular Eye Exams
Regular eye exams are the most effective way to detect glaucoma early. Since symptoms may not appear until significant vision loss has occurred, routine screenings are essential especially for high-risk individuals.
Eye specialists recommend comprehensive eye exams every 1–2 years for adults over 40, or more frequently for those with risk factors. International patients who travel for eye care often benefit from thorough evaluations that may not be readily available in their home countries. Early diagnosis through regular exams can preserve vision and prevent irreversible damage.
⊡ Treatment Options for Glaucoma
Medications
Medications are often the first line of treatment for glaucoma. Prescription eye drops help reduce eye pressure by either decreasing fluid production or improving drainage. These medications must be used consistently, often for life, to prevent further optic nerve damage.
Some patients may experience side effects such as redness, irritation, or changes in heart rate, which should be discussed with an eye specialist. In some cases, oral medications may be prescribed if eye drops alone are insufficient.
For international patients, access to a wide range of modern glaucoma medications and expert guidance abroad can ensure effective pressure control and better long-term outcomes.
Surgery and Other Treatments
When medications are not enough, surgical or laser treatments may be recommended. Laser trabeculoplasty helps improve fluid drainage in open-angle glaucoma, while laser iridotomy is commonly used for angle-closure glaucoma.
Traditional surgeries such as trabeculectomy or minimally invasive glaucoma surgeries (MIGS) create new drainage pathways to lower eye pressure. These procedures can significantly slow disease progression.
Many international patients choose treatment abroad due to access to advanced surgical techniques, experienced ophthalmologists and cost-effective care packages.
⊡ Living with Glaucoma
Living with glaucoma requires ongoing management and lifestyle adjustments. Regular follow-up visits, strict medication adherence and monitoring eye pressure are essential to preserving vision.
Patients should maintain a healthy lifestyle, manage chronic conditions like diabetes and protect their eyes from injury. Emotional support and patient education also play a vital role in coping with a lifelong condition.
International patients often benefit from comprehensive care plans, including follow-up coordination and teleconsultations after returning home, ensuring continuity of care and peace of mind.
⊡ Contact MediKaya Healthcare for GLAUCOMA TREATMENT Support in India
If you are seeking verified information, private hospital options, treatment cost guidance or international patient support Glaucoma treatment in India, our medical coordination team is here to assist you with complete confidentiality and professional care.
MediKaya Healthcare provides end-to-end patient support including hospital selection, doctor consultations, medical visa assistance, treatment coordination and post-treatment follow-up.
📞 WhatsApp & Call: +91 9717998697
📧 Email: info@medikayahealthcare.com
🌐 Website: www.medikayahealthcare.com
Follow us on:
LinkedIn | Instagram | Facebook | Twitter
Our team will respond promptly with verified medical guidance and personalised assistance.